Introduction
Neonatal jaundice is a common condition affecting newborns, especially during the first week of life. Characterized by a yellowish discoloration of the skin and eyes, it occurs due to elevated levels of bilirubin in the blood. While mild jaundice is often harmless and resolves on its own, severe jaundice can lead to serious complications, including brain damage. Phototherapy is a widely used and effective treatment for managing neonatal jaundice. This article provides a comprehensive overview of neonatal jaundice phototherapy, its mechanisms, benefits, and precautions for parents and caregivers.
Definition
Neonatal jaundice phototherapy is a medical treatment used to reduce high levels of bilirubin in a newborn’s blood, which causes yellowing of the skin and eyes. The therapy involves exposing the baby’s skin to a special blue or white light, which helps break down bilirubin into a form that can be more easily eliminated from the body. It is a safe and effective way to prevent complications such as brain damage that can result from severe jaundice.
Understanding Neonatal Jaundice
Bilirubin is a yellow pigment produced during the normal breakdown of red blood cells. In adults and older children, the liver efficiently processes bilirubin, which is then excreted in bile. However, newborns, particularly preterm babies, have immature livers, making it harder for them to process and eliminate bilirubin. This can lead to a condition called hyperbilirubinemia, resulting in jaundice.
Neonatal jaundice can be classified into two types:
- Physiological Jaundice: This is the most common type, usually appearing between 2 to 5 days after birth. It typically resolves within two weeks without treatment.
- Pathological Jaundice: This form appears within the first 24 hours of life or is associated with very high bilirubin levels. Causes include blood type incompatibility (like Rh or ABO incompatibility), infections, liver disorders, or genetic conditions.
Early recognition and treatment of jaundice are crucial to prevent severe complications such as kernicterus, a rare but potentially life-threatening condition caused by bilirubin deposition in the brain.
What is Phototherapy?
Phototherapy is the most commonly used treatment for neonatal jaundice. It involves exposing the baby’s skin to specific wavelengths of light, which helps break down bilirubin into water-soluble forms that can be eliminated through urine and stool. Phototherapy is non-invasive, safe, and highly effective, making it a preferred choice in most neonatal care units.
How Phototherapy Works
The process of phototherapy is based on the principle of photo-oxidation and photo-isomerization. When bilirubin absorbs light in the blue spectrum (wavelengths between 460-490 nm), it undergoes chemical changes:
- Photo-isomerization: Bilirubin changes from a fat-soluble form into a water-soluble form that can bypass the liver and be excreted directly.
- Photo-oxidation: Light exposure also breaks down bilirubin molecules into smaller compounds that can be excreted in urine and feces.
This treatment accelerates the natural process of bilirubin clearance, helping to reduce jaundice levels safely.
Types of Phototherapy
Phototherapy can be administered in several ways, depending on the severity of jaundice:
- Conventional Phototherapy: A fluorescent or LED light is placed above the baby, and the infant is positioned to maximize skin exposure. Eyes are protected with patches, and diapers are kept on to protect sensitive areas.
- Fiberoptic Phototherapy (Bili-Blanket): This involves a light-emitting blanket or pad wrapped around the baby. It is portable and allows parents to hold and feed the baby during treatment, making it convenient for home use.
- Intensive Phototherapy: For severe jaundice, multiple light sources may be used simultaneously, increasing the surface area exposed to light and accelerating bilirubin breakdown.
Preparing for Phototherapy
Before starting phototherapy, healthcare providers assess the baby’s bilirubin levels through blood tests or transcutaneous bilirubinometers. The decision to start phototherapy depends on:
- Baby’s age in hours or days
- Bilirubin levels
- Gestational age
- Presence of risk factors like prematurity or hemolysis
Once phototherapy is recommended, caregivers should be aware of preparation steps:
- Clothing: Babies are usually undressed except for a diaper to maximize skin exposure.
- Eye Protection: Eyes are covered to prevent retinal damage from light exposure.
- Hydration: Phototherapy can increase fluid loss, so frequent feeding (breast milk or formula) is important to prevent dehydration.
- Temperature Monitoring: Babies under phototherapy may experience changes in body temperature, requiring regular monitoring.
Duration of Phototherapy
The duration of phototherapy varies depending on bilirubin levels, response to treatment, and the baby’s overall health. Typically, phototherapy continues until bilirubin levels drop to safe limits. Frequent monitoring ensures the baby receives adequate treatment without overexposure.
- Mild to Moderate Jaundice: Phototherapy may last 24–48 hours.
- Severe Jaundice: Intensive or prolonged therapy may be required, sometimes combining conventional and fiberoptic methods.
Benefits of Phototherapy
Phototherapy offers several advantages in managing neonatal jaundice:
Non-invasive: Unlike blood transfusions or other invasive treatments, phototherapy is gentle and pain-free.
Highly Effective: Most cases of moderate jaundice respond well within 24–72 hours.
Reduces Risk of Complications: Timely treatment prevents severe neurological damage associated with high bilirubin levels.
Flexible Administration: Portable fiberoptic devices allow for home treatment in suitable cases.
Potential Side Effects
While phototherapy is generally safe, some side effects may occur:
Skin Rash or Irritation: Some babies develop mild redness or rashes.
Dehydration: Increased fluid loss may require more frequent feeding.
Eye Damage: Rare, but improper eye protection can harm the eyes.
Temperature Fluctuations: Babies may get too warm or cold under the lights.
These risks are minimal when phototherapy is administered under proper medical supervision.
Home Phototherapy: Is it Safe?
Home phototherapy with fiberoptic blankets is sometimes recommended for mild jaundice in stable infants. While convenient, parents must follow strict instructions regarding:
Proper placement of the blanket
Ensuring constant contact between the baby’s skin and the light pad
Monitoring for signs of dehydration, overheating, or irritability
Scheduling follow-up bilirubin checks
Professional guidance is essential to ensure effectiveness and safety.
Supporting Your Baby During Phototherapy
Parents play a crucial role in ensuring phototherapy is successful:
Frequent Feeding: Adequate hydration helps eliminate bilirubin through urine and stool.
Skin Care: Check for rashes or irritation and report any concerns to the healthcare team.
Bonding: Use moments when the baby is not under lights for skin-to-skin contact and gentle interaction.
Monitoring: Keep track of temperature, feeding patterns, and overall behavior to report to the medical team.
When to Seek Immediate Medical Attention
Although phototherapy is highly effective, parents should seek immediate help if:
Jaundice worsens or spreads rapidly
Baby becomes lethargic or refuses to feed
Signs of dehydration, such as dry mouth or fewer wet diapers, appear
Unusual symptoms like fever or vomiting develop
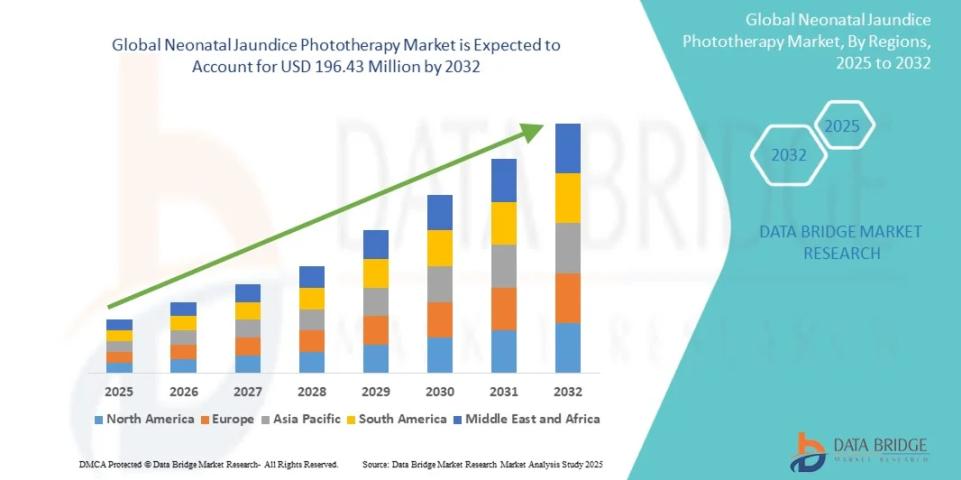
Growth Rate of Neonatal Jaundice Phototherapy Market
According to Data Bridge Market Research, the size of the global neonatal jaundice phototherapy market was estimated at USD 115.50 million in 2024 and is projected to grow at a compound annual growth rate (CAGR) of 6.86% to reach USD 196.43 million by 2032.
Learn More: https://www.databridgemarketresearch.com/reports/global-neonatal-jaundice-phototherapy-market
Conclusion
Neonatal jaundice is a common and generally manageable condition, but early detection and proper treatment are critical. Phototherapy remains the cornerstone of treatment, offering a safe and effective method to reduce bilirubin levels and prevent serious complications. Parents and caregivers play an essential role in supporting their baby through phototherapy by ensuring proper feeding, monitoring for side effects, and maintaining close communication with healthcare providers.