Medical insurers that work with legacy claims systems experienced higher processing times, increased staff workloads, and slow payment completion. Healthcare claims processing systems designed for modern demands addresses fundamental problems..
Total and Permanent Disability (TPD) insurance is designed to provide financial protection when an illness or injury prevents you from ever working again in your usual occupation or any suitable..
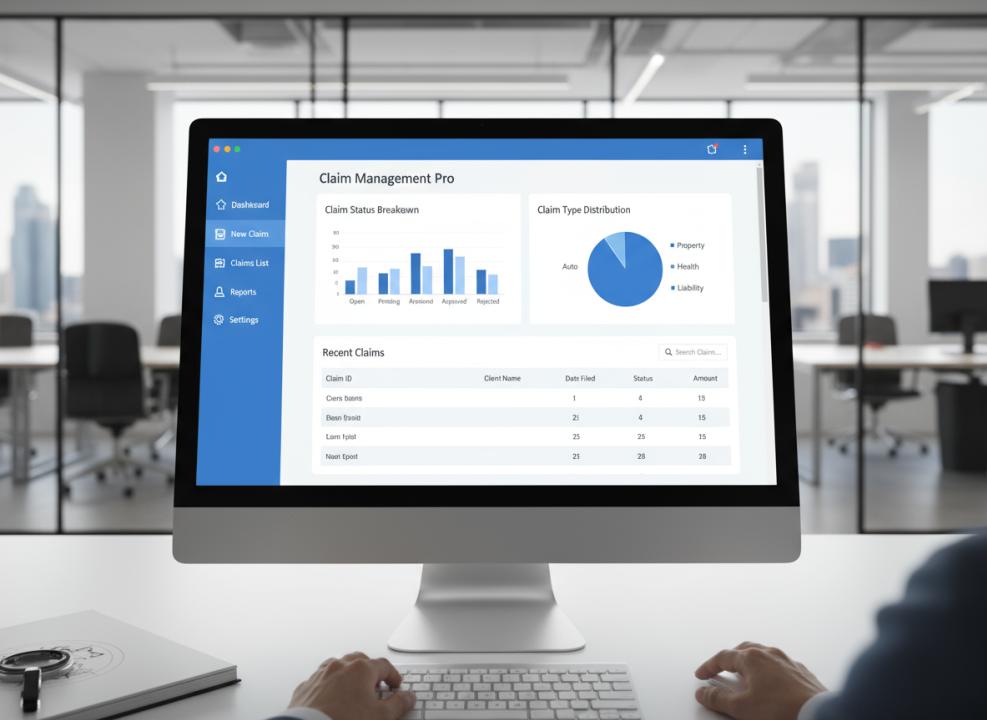
The claims process serves as the moment of truth between insurers and policyholders. Software powering this process must deliver operational efficiency and exceptional customer experiences. Companies that successfully implement the..
Regulatory compliance becomes seamless with built-in workflow checks. Insurance claims adjuster software maintains unalterable digital audit trails, documenting every decision and action taken during claims processing. This automatic documentation eliminates..
Claims processing success depends on customer trust. Policyholders expect clear explanations when filing claims, especially during stressful situations. Explainable AI insurance claims processing software delivers this transparency while maintaining processing..
Automation makes every claim processing step more efficient from the first notice of loss to final payment. The automated claims processing insurance solutions handle routine cases without human intervention. This..
The right claims automation solution delivers advantages that extend beyond basic efficiency improvements. Fraud detection capabilities in automated claims processing solutions improve significantly when advanced algorithms analyze claim patterns. Staff..
Revolutionize payer operations with AI-powered healthcare claims management software that enhances claims accuracy, minimizes denials, and accelerates settlements — delivering a seamless experience for payers while reducing administrative burdens.Streamline claims..
The future of global insurance depends on how effectively companies can navigate regulatory differences across borders. Claims processing automation represents a strategic necessity for insurers with international ambitions. Companies that..
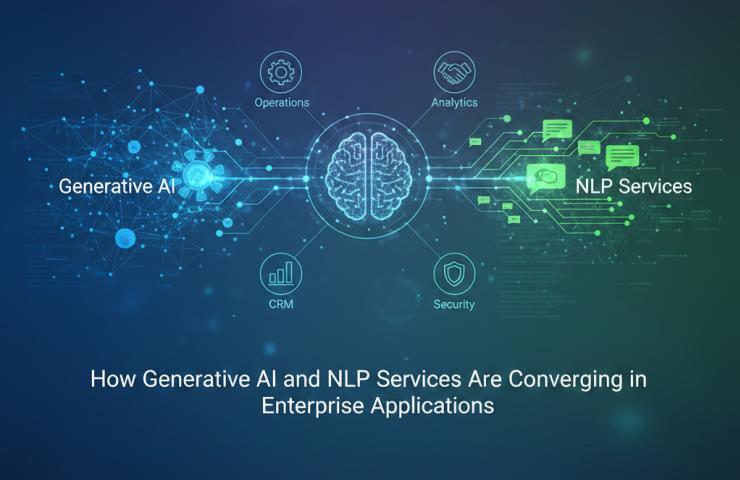
Enterprises are experiencing a rapid shift in how digital systems understand and generate human language. As global teams manage larger volumes of unstructured data, the connection between generative intelligence and..
In the rapidly growing Software-as-a-Service (SaaS) industry, payment processing means more than just accepting credit cards. It is essential for generating recurring revenue, keeping customers, and scaling globally. Efficient SaaS..
Medical insurers that work with legacy claims systems experienced higher processing times, increased staff workloads, and slow payment completion. Healthcare claims processing systems designed for modern demands addresses fundamental problems..
Intelligent Document Processing Industry Outlook:Straits Research has added a report titled “Global Intelligent Document Processing Market Professional Report 2025-2033” to its database of research reports. The study provides complete details..
Claims processing success depends on customer trust. Policyholders expect clear explanations when filing claims, especially during stressful situations. Explainable AI insurance claims processing software delivers this transparency while maintaining processing..
Automation makes every claim processing step more efficient from the first notice of loss to final payment. The automated claims processing insurance solutions handle routine cases without human intervention. This..
Comprehensive Guide to Setting Up a Cinnamon Oil Processing Plant:IMARC Group’s Cinnamon Oil Processing Plant Analysis Report 2025 offers a complete roadmap to successfully establish a cinnamon oil processing plant...
The right claims automation solution delivers advantages that extend beyond basic efficiency improvements. Fraud detection capabilities in automated claims processing solutions improve significantly when advanced algorithms analyze claim patterns. Staff..
Natural language processing services from WebClues Infotech help businesses work smarter with text and voice data. As a natural language processing company, we design solutions that interpret sentiment, detect intent,..