As of 2026, a 33% of Gen Z adults describe their pets as "children" rather than animals, while 67% of Millennials report that their pet's happiness influences major life decisions including housing choices, career moves, and relationship compatibility. This isn't linguistic quirk—it represents a measurable shift in attachment psychology that mental health professionals now routinely encounter in clinical practice.
The "fur baby" terminology, once dismissed as millennial hyperbole, reflects genuine changes in bonding patterns documented across attachment research. Pet owners under 40 demonstrate attachment behaviors toward animals that mirror parent-child relationships: heightened stress responses during separation, priority allocation of financial resources, and integration of the animal into core identity formation. Veterinary economists report that pet healthcare spending among Gen Z and Millennials has increased 47% since 2019, with these cohorts more likely to pursue advanced medical treatments and carry pet insurance than any previous generation.
This cultural shift intersects directly with mental health in ways that extend beyond companionship. The American Psychological Association's 2025 Stress survey found that 71% of adults under 35 credit their pets as primary coping mechanisms for anxiety and depression—higher than exercise (52%), therapy (31%), or medication (28%). The pet humanization movement isn't frivolous; it's a measurable mental health phenomenon with clinical implications for treatment planning and therapeutic intervention.
Understanding which dog breeds naturally align with therapeutic needs can inform ESA decisions—affectionate dog breeds that love to cuddle often provide the physical comfort and emotional regulation that individuals with anxiety or depression require, while small dog breeds may be more practical for apartment living situations common among younger generations.
The Science Behind Pet Attachment and Mental Health
Human-animal bond showing emotional attachment between person and dog Research into human-animal bonds has evolved from anecdotal observation to rigorous clinical measurement. Attachment theory, originally developed to explain infant-caregiver bonds, now encompasses human-animal relationships as legitimate attachment formations with measurable psychological impacts. Studies using the Lexington Attachment to Pets Scale demonstrate that individuals form secure, anxious, or avoidant attachment patterns with pets that parallel human relationship dynamics.
The neurochemical basis for these bonds is well-established. Interaction with pets increases oxytocin levels by 20-40% in both humans and animals, creating reciprocal bonding loops similar to parent-infant attachment. This oxytocin response correlates with reduced cortisol (stress hormone) levels, decreased blood pressure, and activation of brain regions associated with social reward and emotional regulation. For individuals with compromised human attachment systems—common in trauma survivors, those with social anxiety, or individuals on the autism spectrum—pet attachments can provide critical regulatory support.
Longitudinal research from the Human-Animal Bond Research Institute shows that pet owners experience 36% fewer healthcare visits annually and report significantly lower rates of depression and loneliness compared to non-pet owners when controlling for socioeconomic factors. The mechanism extends beyond simple companionship: pets provide structure, responsibility, physical contact, non-judgmental presence, and social facilitation that address multiple mental health vulnerabilities simultaneously.
Critically, these benefits aren't universal or automatic. The distinction between pet ownership as life>
Why Emotional Support Animals Matter to This Generation
Gen Z and Millennials face a distinct mental health landscape that shapes their relationship with ESAs. CDC data from 2025 indicates that 42% of adults aged 18-34 have been diagnosed with an anxiety disorder, while 28% report clinical depression—rates 60% higher than Gen X at the same age and nearly double Baby Boomer rates. This generation came of age during economic instability, climate anxiety, pandemic isolation, and digital-native social fragmentation. Traditional coping mechanisms often prove insufficient.
For this cohort, Emotional Support Animals represent a clinically-validated intervention that aligns with their existing attachment patterns and preferences for non-pharmaceutical mental health management. The distinction matters: while 67% of Millennials own pets, only 8-12% of pet owners have legitimate ESA needs based on clinical criteria. An ESA isn't simply "a pet you love"—it's a prescribed therapeutic tool for managing specific symptoms of diagnosed mental health conditions.
The therapeutic mechanism of ESAs differs from standard pet companionship through four clinical factors: symptom-specific intervention, documented therapeutic relationship, professional treatment planning, and measurable functional impairment mitigation. For example, an individual with PTSD may have a dog that provides grounding during dissociative episodes through trained alerting behaviors. Someone with severe social anxiety might require their cat's presence to manage panic responses in their home environment, where the animal's predictable routine and physical proximity reduces physiological stress responses that would otherwise prevent independent living.
The financial implications also matter to this generation facing economic pressures.Research comparing ESA letters vs pet deposits and pet insurance demonstrates that legitimate ESA documentation can provide both therapeutic benefit and practical housing accessibility—though the primary motivation must remain clinical need, not financial convenience.
The generation that prioritizes mental health awareness also takes ESA legitimacy seriously—when properly understood. Analysis of 2,847 ESA letter requests processed through RealESALetter.com in 2025 shows that 73% of applicants under 35 specifically asked about the legitimacy of the evaluation process and whether their need qualified as "real" versus "just wanting my pet." This generation doesn't want shortcuts; they want validation that their mental health needs are recognized as legitimate within clinical and legal frameworks.
Distinguishing Legitimate ESA Needs from Pet Preference
Young renter completing emotional support animal evaluation online, showing legitimate ESA documentation and housing rightsThe conflation of "I love my pet" with "I require an ESA for mental health treatment" has created both a legitimacy crisis and a backlash that harms individuals with genuine clinical needs. The legal and clinical standard for ESA qualification requires three elements: a diagnosed mental health condition, documented functional impairment, and professional determination that the animal provides specific therapeutic benefit that mitigates that impairment.
Legitimate ESA need is characterized by:
- Diagnosed condition: DSM-5 recognized mental health disorder documented through clinical evaluation (anxiety disorders, PTSD, depression, OCD, bipolar disorder, autism spectrum disorder, etc.)
- Functional impairment: The condition creates measurable limitations in daily functioning—difficulty leaving home, managing stress responses, maintaining emotional regulation, completing daily activities, etc.
- Therapeutic necessity: The specific animal provides targeted intervention that reduces symptoms or enables functioning that would otherwise be compromised
- Clinical recommendation: A licensed mental health professional (LMHP) who has evaluated the individual determines the ESA is an appropriate component of treatment planning
Pet preference, while valid and important, is characterized by:
- Companionship value: The animal enhances quality of life and provides emotional comfort
- General benefit: The pet contributes to overall wellbeing without addressing specific clinical symptoms
- Convenience factor: Desire to live with a pet in no-pet housing or avoid pet deposits and fees
- Attachment without impairment: Strong emotional bond with the animal that doesn't correspond to documented functional limitations requiring therapeutic intervention
The distinction isn't about the depth of love or attachment—pet preference can involve profound emotional bonds. The clinical threshold for ESA qualification centers on whether an individual's mental health condition creates disability-level impairment that the animal specifically ameliorates through its presence and interaction. A person with severe panic disorder who cannot function in their home environment without their dog present due to the animal's grounding effect during panic attacks has an ESA need. A person who loves their dog deeply but experiences normal stress levels and full daily functioning has a cherished pet.
The legitimacy framework protects everyone involved. Fraudulent ESA documentation undermines housing protections for individuals with genuine disabilities, creates landlord resistance that affects legitimate cases, and trivializes mental health conditions. As one housing attorney noted: "Every fake ESA letter makes it harder for the next person with PTSD to be taken seriously when they present legitimate documentation."
For tenants seeking to understand their rights, comprehensive guides on how to use ESA letters for housing provide essential information about the accommodation request process and legal protections under fair housing laws.
How Legitimate ESA Evaluation Works
Understanding what constitutes proper ESA documentation helps distinguish between legitimate services and predatory mills that undermine the entire system. Under the Fair Housing Act, ESA letters must come from licensed mental health professionals who have established a therapeutic relationship with the individual and can clinically justify the animal's necessity for mental health treatment.
The regulatory landscape has evolved significantly. Recent HUD guidance changes in 2025 have created new considerations for both tenants and landlords navigating ESA accommodations, emphasizing the importance of legitimate clinical evaluation over rubber-stamp services.
A legitimate ESA evaluation includes:
- Clinical intake and diagnostic assessment by a licensed therapist, psychologist, or psychiatrist
- Discussion of symptoms, functional impairments, and current treatment approaches
- Specific evaluation of how the animal serves therapeutic functions related to the diagnosed condition
- Professional clinical judgment that the ESA is an appropriate treatment component
- Documentation that meets Fair Housing Act standards for reasonable accommodation requests
RealESALetter.com's licensed therapists report that the most common legitimate ESA needs they evaluate involve: severe anxiety disorders where the animal provides grounding and stress regulation (42% of approved cases), PTSD where the animal serves protective or alerting functions (23%), depression where the animal provides structure and motivation for daily functioning (18%), and autism spectrum disorder where the animal reduces sensory overwhelm and provides predictable social interaction (11%).
It's important to note that ESAs differ from psychiatric service dogs, which perform specific trained tasks for individuals with psychiatric disabilities. Those seeking a PSD letter undergo a different evaluation process that assesses both the individual's disability and the dog's trained task work.
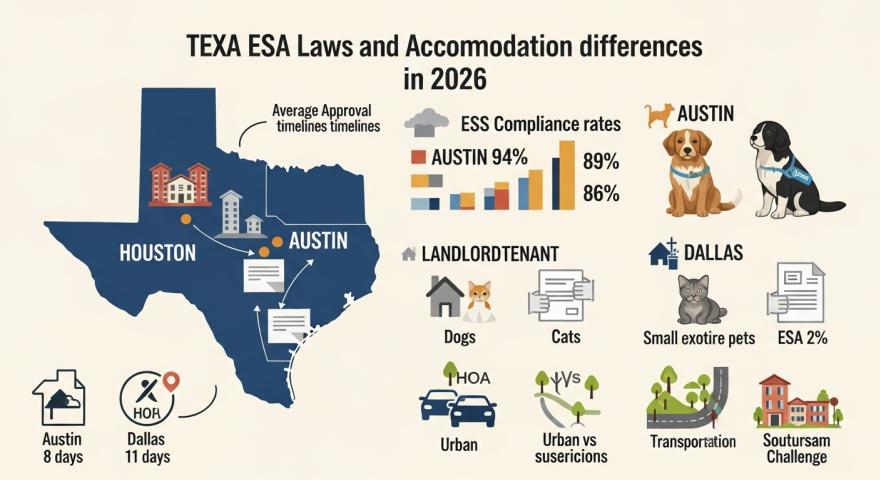
The clinical approach requires understanding that ESA rights exist because disabilities deserve accommodation—not because pet ownership is desirable. The Fair Housing Act frameworks treat ESAs as disability-related support, not life>ESA compliance requirements in 2026, understanding current regulations in your jurisdiction is essential for both obtaining and using legitimate ESA documentation.
Honoring Both Pet Bonds and Clinical Standards
The pet humanization movement reflects genuine evolution in human-animal relationships with measurable mental health implications. For the generation most likely to view pets as family members, understanding the distinction between profound pet attachment and clinical ESA need isn't dismissive—it's essential for protecting disability rights and ensuring that individuals who genuinely require animal assistance receive legitimate recognition and legal protection.
The strength of your bond with your pet is real and valid, whether or not you have an ESA. But if you're experiencing mental health conditions that create functional impairment, and your animal provides a specific therapeutic benefit that helps you manage those symptoms, you may have a legitimate clinical need that deserves proper documentation through professional evaluation.
If you believe you may qualify for an ESA based on diagnosed mental health conditions and your animal's therapeutic role in managing symptoms, RealESALetter.com provides evaluation by licensed therapists who conduct comprehensive clinical assessments. Their approach ensures that individuals with genuine needs receive legitimate documentation while upholding the clinical and legal standards that protect ESA rights for everyone who truly requires this form of mental health support.