Bone tumor reconstruction is one of the most complex challenges in orthopedic oncology. Surgeons are not only required to remove the tumor completely but also to restore bone structure, function, and patient quality of life. Traditional reconstruction methods often involve standardized implants that may not perfectly fit the patient’s anatomy, leading to complications, longer recovery, and compromised outcomes.
This is where patient specific implants are creating a paradigm shift. Leveraging advanced imaging, digital planning, and 3D printed medical implantstechnology, companies like Curewith3D are transforming how bone tumor reconstruction is approached—making it more precise, predictable, and patient-centered than ever before.
Understanding Bone Tumor Reconstruction Challenges
Bone tumors, whether benign or malignant, often require aggressive surgical intervention. After tumor resection, surgeons are left with large bone defects that must be reconstructed to restore stability, mobility, and limb function.
Traditional reconstruction techniques typically rely on:
Standard modular implants
Bone grafts or allografts
Generic fixation plates
While effective in some cases, these methods can struggle with complex anatomy, irregular bone loss, and alignment issues. This mismatch can increase the risk of implant failure, infection, and revision surgery.
What Are Patient Specific Implants and Why Do They Matter?
Patient specific implants are custom-designed medical implants created using a patient’s CT or MRI scan data. Instead of adapting the patient to the implant, the implant is designed to match the patient—precisely.
Using 3D printed medical implants, Curewith3D develops reconstruction solutions tailored to:
Exact bone geometry
Tumor defect size and shape
Load-bearing requirements
Surgical approach
This level of personalization is particularly critical in bone tumor reconstruction, where no two defects are the same.
How Curewith3D Uses Technology to Transform Reconstruction
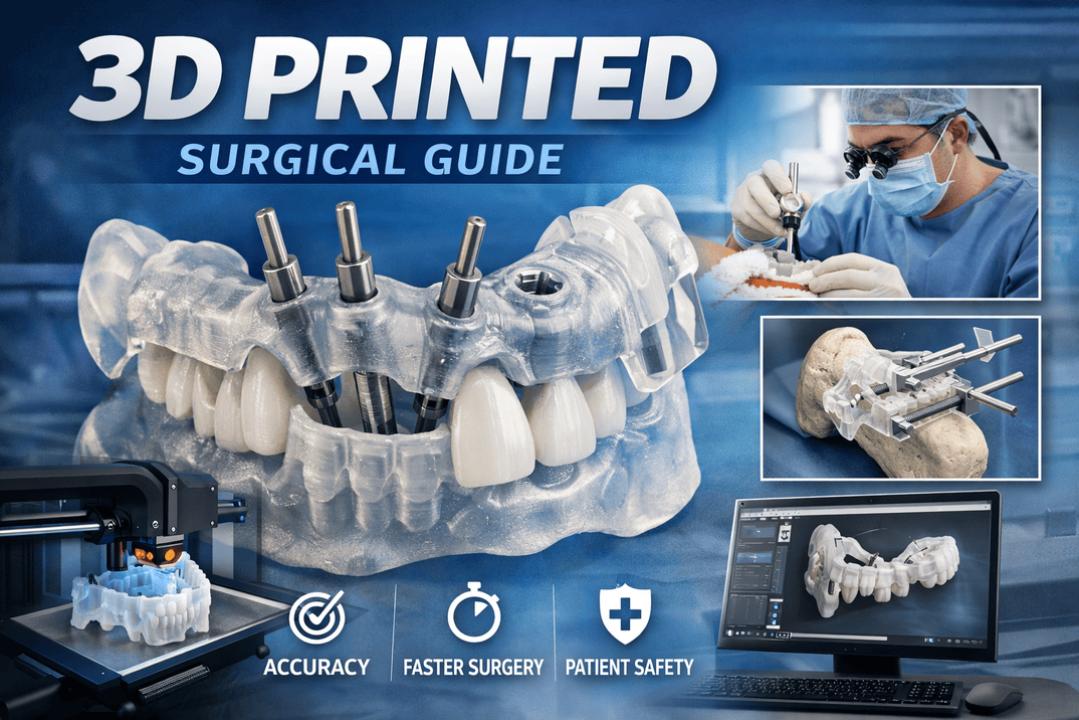
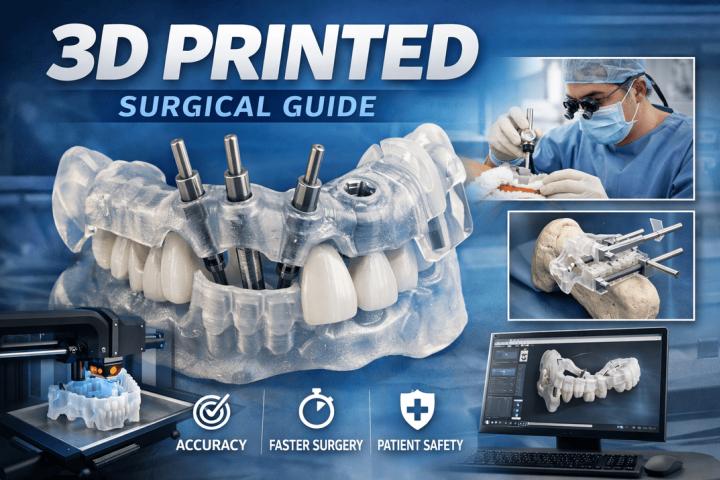
Curewith3D combines medical imaging, digital engineering, and additive manufacturing to deliver advanced orthopedic solutions. The workflow typically includes:
High-resolution imaging to capture anatomy
Virtual surgical planning with oncologic surgeons
Custom implant design based on biomechanical analysis
3D printing using biocompatible materials such as titanium
Rigorous quality and safety validation
This integrated approach significantly improves surgical accuracy and predictability.
Key Benefits of Patient Specific Implants in Bone Tumor Reconstruction
1. Superior Fit and Accuracy
Custom implants align perfectly with the remaining bone, reducing gaps and stress points. This precision is critical for long-term stability and function.
2. Reduced Surgery Time
Pre-planned implants and cutting guides minimize intraoperative adjustments. Studies show that patient specific solutions can reduce operating time by 20–30%, lowering anesthesia-related risks.
3. Faster Recovery and Rehabilitation
Better fit means less trauma to surrounding tissue, enabling earlier mobilization and quicker functional recovery.
4. Improved Limb Salvage Rates
Customized reconstruction increases the success of limb-sparing surgeries, which are now performed in over 85% of bone tumor cases globally.
5. Lower Risk of Revision Surgery
Accurate load distribution and stable fixation reduce implant loosening and mechanical failure.
Common Questions About Patient Specific Implants in Bone Tumor Cases
Are patient specific implants safe for cancer patients?
Yes. These implants are made from medical-grade, biocompatible materials and meet international regulatory standards. They are designed to integrate with bone while maintaining structural integrity.
How long does it take to manufacture a custom implant?
With advanced workflows like those at Curewith3D, implants can be designed and manufactured within 2–4 weeks, depending on complexity.
Do patient specific implants work for children and young adults?
Yes. Customization is especially valuable in younger patients, where preserving anatomy and function is crucial for long-term outcomes.
Are these implants more expensive?
While initial costs may be higher, reduced surgery time, fewer complications, and lower revision rates often make patient-specific implants more cost-effective over time.
Clinical Impact and Real-World Outcomes
Clinical data increasingly supports the use of patient specific implants in orthopedic oncology. Research indicates:
Improved implant survival rates
Better functional scores post-surgery
Higher patient satisfaction
By addressing anatomical complexity directly, Curewith3D helps surgeons achieve predictable results even in the most challenging reconstruction cases.
The Future of Bone Tumor Reconstruction with Curewith3D
The future of orthopedic oncology lies in personalization. Emerging trends include:
AI-assisted implant design
Smart implants with monitoring capabilities
Bioactive surfaces to promote faster bone integration
Curewith3D is actively advancing these innovations, positioning itself at the forefront of next-generation bone tumor reconstruction.
Conclusion
Patient specific implants are no longer a niche innovation—they are rapidly becoming the gold standard in bone tumor reconstruction. By combining precision engineering, advanced 3D printed medical implants, and collaborative surgical planning, Curewith3D is transforming outcomes for patients facing some of the most complex orthopedic challenges.
For surgeons, this means greater confidence and control. For patients, it means faster recovery, better function, and renewed quality of life. The transformation is not coming—it’s already here.