Tooth loss in the upper jaw is not always a simple problem to fix. In many patients, long-term tooth loss, periodontal disease, or trauma leads to significant bone loss in the upper jaw, making conventional dental implant placement difficult. This condition often leaves clinicians with a critical decision to make: rebuild the lost bone using grafting techniques, or bypass the problem entirely with advanced solutions like zygoma implants.
Both approaches are well-established in modern implant dentistry, yet they are recommended for very different anatomical situations and patient needs. Choosing the right method depends not just on the number of missing teeth, but on the quality, volume, and structure of the remaining maxillary bone.
Before comparing bone grafting and zygoma implants in detail, it is essential to understand the underlying condition that makes these interventions necessary in the first place.
What is Atrophic Maxilla?
Bone loss in the upper jaw can occur due to long-term tooth loss, periodontal disease, trauma, tumors, or failed implants. Over time, the maxillary bone resorbs and the maxillary sinus expands, leaving insufficient bone height and density for standard dental implants.
What Is Bone Grafting in Dental Implantology?
Bone grafting is a surgical procedure that rebuilds or augments deficient jawbone to create a stable foundation for implants. Grafting material may be sourced from the patient (autograft), a donor (allograft), animal sources (xenograft), or synthetic materials.
How Bone Grafting Works
The graft material is placed in areas of bone deficiency and allowed to integrate with the existing bone over several months. Once sufficient bone volume is achieved, dental implants can be placed.
Clinical Advantages
Bone grafting allows clinicians to place implants in anatomically familiar positions. It has a long history of clinical use and is suitable for mild to moderate bone loss.
Clinical Limitations
In cases of severe maxillary atrophy, bone grafting may require multiple surgeries, longer healing times, and carries a higher risk of graft resorption or failure. Treatment timelines can extend from 9 to 18 months before final prosthetic rehabilitation.
What Are Zygoma Implants?
A zygoma implant is a long dental implant anchored in the zygomatic bone (cheekbone) rather than the maxillary bone. The zygomatic bone has dense cortical structure, making it a reliable anchorage point even in patients with extreme maxillary bone loss.
Originally developed for patients with maxillary defects following tumor surgery, zygoma implants are now widely used in implant rehabilitation for severely atrophic maxillae.
How Zygoma Implants Work
Instead of rebuilding the jawbone, zygoma implants bypass the deficient maxilla entirely. The implant is placed at an angle, extending from the oral cavity into the zygomatic bone, often allowing immediate or early loading.
Bone Grafting vs Zygoma Implants
Surgical Approach
Bone grafting focuses on reconstructing lost bone before implant placement. Zygoma implants avoid grafting altogether by using existing facial bone structures. As a result, zygoma implant surgery is technically more complex but often involves fewer overall procedures.
Treatment Duration
Bone grafting requires extended healing periods before implants can be placed. Zygoma implants often enable faster rehabilitation, sometimes allowing immediate fixed prostheses, which can be a significant advantage for patients seeking quicker results.
Predictability and Stability
In severe atrophic cases, graft resorption can compromise outcomes. Zygoma implants benefit from the high density of the zygomatic bone, offering strong primary stability and predictable anchorage when placed by experienced clinicians.
Patient Morbidity
Bone grafting may involve donor site surgery and prolonged discomfort. Zygoma implant placement is a single-stage surgical procedure but requires advanced surgical expertise and careful anatomical planning.
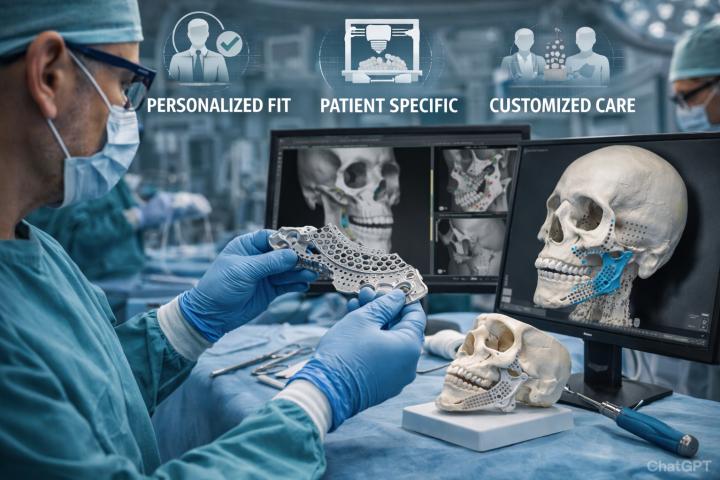
Role of Digital Planning and 3D Technology
Modern implant dentistry increasingly relies on digital workflows to improve safety and precision. 3D dental implants planning using CBCT scans allows clinicians to evaluate bone anatomy, sinus position, and zygomatic structure accurately.
With 3D printed dental implants and patient-specific surgical guides, implant placement can be planned virtually before surgery. This improves angulation accuracy, reduces surgical time, and enhances predictability—especially critical in complex zygoma implant cases where anatomical margins are narrow.
Indications: Which Approach Works Better?
Bone grafting is generally suitable for patients with mild to moderate bone loss who can tolerate longer treatment timelines. It may also be preferred when anatomical conditions allow predictable graft integration.
Zygoma implants are often the preferred option for patients with severe maxillary atrophy, failed grafts, or those who wish to avoid multiple surgeries. They are particularly beneficial when conventional dental implants are not feasible despite grafting attempts.
Risks and Considerations
Both treatments carry surgical risks, including infection, sinus complications, and implant failure. Zygoma implants require precise surgical execution due to proximity to vital structures such as the orbit and sinus cavity. Therefore, clinician experience and proper digital planning are critical.
Patients must undergo thorough clinical and radiographic evaluation before deciding on either approach. Individual health conditions, bone anatomy, and long-term expectations all influence treatment success.
Conclusion
When treating the atrophic maxilla, there is no one-size-fits-all solution. Bone grafting and zygoma implants each play an important role in advanced implant dentistry. While bone grafting remains effective for select cases, zygoma implants have emerged as a reliable, time-efficient alternative for patients with severe bone loss.
Advancements in 3D dental implants, digital planning, and 3D printed dental implants continue to improve outcomes for both approaches. Ultimately, the choice between bone grafting and zygoma implants should be guided by careful diagnosis, evidence-based planning, and patient-specific needs.
A well-informed decision—made collaboratively between clinician and patient—leads to safer treatment, predictable outcomes, and long-term oral rehabilitation.