In the 21st century, the health insurance industry is experiencing more change in comparison to the last century. It is no surprise that policyholders' in this industry want a quick response rate, the ability to pay their bill or submit a claim through a digital experience, and overall a personalized experience whether it is in-person or digital. On the other hand, the pressure of managing complex processes like managing thousands of policies, managing claims, and strict compliance is an incredibly complex and overwhelming job. This is where the CRM software for health insurance companies can help you out!
A CRM (customer relationship management) system not only stores customer details. It can provide the insurers with a 360-degree view of each policyholder, which allows agents and teams to serve policyholders with the right service at the right moment. The CRM will produce efficiencies from the simplest things like tracking claims and even an automated renewal reminder. Additionally, the health insurance CRM software assists with practical efficiency that builds "brand love" and checks every important matter for your customers.
It gets even better, with each product offering, your business will remain compliant with industry regulations like HIPAA, GDPR, while not sacrificing frictionless experience for your customers. CRM is quickly transitioning from a must-have to a critical way to deliver customer service and industry operational excellence in health insurance.
In this blog post we will break down key features to consider when shopping for health insurance CRM software and what the right system can mean for your business. Let’s check in detail!
Why Do Health Insurance Companies Need a CRM?
Health insurance can be complicated. Policies, renewals, and claims all require accuracy and care. At the same time, today’s consumers expect fast, digital-first, and highly personalized experiences, which is where health insurance CRMs come into play. Some of the top reasons are as follows:
Meet rising expectations: Policyholders want to have access to all their policy details, claim status, and personalized recommendations, instantly. A health insurance CRM makes this easy with automated reminders and self-service options as well as 24/7 access for communication.
Simplifying policy and claims management: Instead of managing spreadsheets and other manual processes, a CRM for health insurance centralizes customer and policy data, making the renewal and claims processes easier for both agents and customers.
Ensures compliance and security: Institutions need to access and share sensitive information that are protected by regulations like HIPAA and GDPR. Health insurance CRMs often have protections built into the platform to safeguard sensitive health and financial data.
Retention and cross selling: Without being intrusive, CRMs can track customer behaviors, preferences, and needs so insurers can determine upsell opportunities and keep their customers engaged with their service and products for the long-term.
In summary, a health insurance CRM provides an opportunity to gain competitive advantage for health insurers to delight their customers with better service, less errors, and foster customer loyalty for the long-term.
Essential Features to Look for in Health Insurance CRM Software
Selecting the best CRM for your health insurance company is more than just checking off boxes. It’s identifying a system that will simplify your work, please your customers, and streamline your processes. Let’s check the top features that are essential for health insurance CRM software!
1. Policy & Customer Management
Policy and customer management is the most essential feature of any insurance CRM. Imagine a single centralized data source in which all details about the file holder including personal information, types of policy, payment history, dependents, and prior claims are organized in one easy to reference location.
Your agents will not have to sort through files or spreadsheets to access a customer’s entire history at their fingertips.
Renewals and premium payments will be a breeze to track, reducing the likelihood of missing due dates.
Customer segmentation can be based on demographics, policy type, or health needs all allowing for easy outreach and personal offers.
2. Management of Leads and Sales Pipeline
The health insurance industry is a competitive one, and leads are worth their weight in gold. Your CRM should not only track leads. It should help you nurture leads through all phases of the sales funnel.
Leads can come from multiple sources, such as website inquiries, social media, call centers, or referral sources. Your CRM keeps leads organized together in one central customer relationship management platform.
The CRM workflow automation can effectively manage lead follow-up, quotes, and onboarding, ensuring that nothing falls through the cracks.
Sales teams can project revenue, measure agent performance, and find out which campaigns lead to conversions. As a result, it keeps your sales pipeline healthy, predictable, and scalable.
3. Claims Management
Claims is where customers are often most stressed, how you handle claims can make or break your relationship with the customer. Using a CRM with claims management functionality takes the stress out of claims submission!
By creating a digital claims submission option to eliminate paperwork and lengthy waiting times, customers can always have peace of mind.
Your CRM will integrate into third-party systems for claims verification and approval of claims. For example, hospitals and TPAs, to expedite the claims process.
As a bonus, your customers will get real-time status updates on their claims, no more tracking down your adjuster by phone!
Streamlining claim management will improve customer satisfaction and build confidence and trust in your brand.
4. Process Automation and Workflow Management
We can all agree that manual processes can feel like a drag on time and can increase the frequency of human error.
In this case, automation can be a real game changer. Renewal reminders, premium due dates, and follow-up emails can each be fully automated.
Claims can flow through a pre-defined approval workflow, and escalations can even be built into the process where needed. Routine processes that took a team member hours of manual effort can now be completed in minutes, giving them time back to focus on higher-value work.
Smart automation streamlines processes, reduces inaccuracies, and ensures an even process providing customers with a better experience.
5. Omnichannel Communication
Your customers do not just exclusively use one communication channel. Sometimes they prefer email, other times they may send you a quick WhatsApp message or perhaps even just call you. A modern CRM merges all of these touchpoints into one communication center.
Regardless of whether it is an email, SMS, or a live chat or call center, everything is tracked and logged. AI chatbots offer the most instant referral option and common questions about a policy or create a claim in a text conversation as right as the conversation happens, providing 24/7 response.
Using a personalized communication template to ensure a personal touch makes the message feel much more human and specific. This consistency also makes your company easier to contact and appear more reliable to the customer.
6. Analytics and Reporting
Data is powerful, but only if you can easily understand it. A health insurance CRM that includes analytics and reporting features enables you to make informed decisions.
Visual dashboards provide quick access to sales performance, claims ratios, and customer satisfaction.
Predictive analytics identify which customers are in jeopardy of leaving, allowing you to retain them.
Built-in compliance reporting ensures you are audit-ready.
Having these insights allows you to not just react but to proactively better your business strategy.
7. Regulatory Compliance and Data Security
Few industries face as much sensitivity regarding data than health insurance. That is why features for compliance and security are not optional; they are mandatory.
Top CRMs are structured with HIPAA, GDPR, and other regional regulations in mind. Data encryption and role-based access control protects data from breach.
Every customer engagement is tracked, offering visibility and supporting accountability.
Hence, it not only keeps regulators satisfied, but also gives customers confidence that their data is well protected.
Final Thoughts
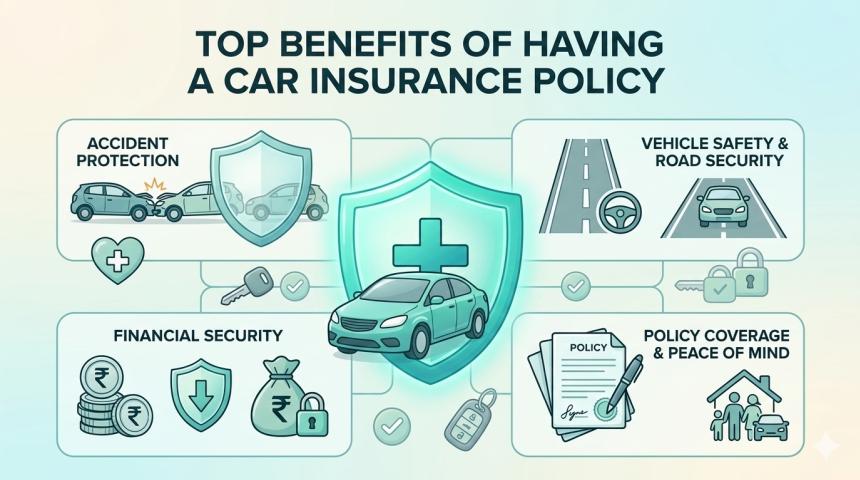
In the fast-paced world of health insurance, there is no substitute for customer trust and uninterrupted operations. A modern CRM system helps insurers achieve both goals through customer data centralization, automation of routine tasks, and the streamlining of claims processes to ensure compliance. As insurers look to become more efficient, they can focus on the new digital-first experiences brand new customers expect, and look to past customers to improve upon.
The right health insurance CRM software should be considered more than an efficiency tool, it should be considered a more strategic investment. This is realized by selecting a health insurance CRM software equipped with the solid features like policy management, automated claims, omnichannel communication, analytics, and AI. Selecting the right vendor will help you to retain current customers, grow your revenue, and keep you above the competition. In essence, a CRM system serves as the missing bridge between efficient operational performance and providing exceptional customer service.